
The number of people hospitalized around Alaska with the disease caused by the coronavirus is still somewhat low compared to other states — only 23 as of Monday.
Most patients who test positive for the disease are sent home to isolate themselves. But that’s going to change as the number of COVID-19 cases go up.
At Juneau’s Bartlett Regional Hospital, staff are already preparing for a potential spike in coronavirus patients.
Stories of the COVID-19 pandemic in Lower 48 hospitals include doctors, nurses and first responders falling victim to the disease.
There’s also been the ongoing shortage of medical supplies like ventilators, masks and gowns.
And hospitals have been overwhelmed by a big surge in patients.
In Juneau, Nicole Skeek-Wheeland has similar concerns about Bartlett Regional Hospital. She worries if she gets the virus, she’ll likely end up there. After lung infections requiring a barrage of antibiotics, she’s left with a very weak immune system.
That makes her especially upset when she sees people on social media not taking the coronavirus seriously and claiming “that this is just a big hoax,” she said.
“‘This isn’t real. Don’t believe in science. Pray and send good thoughts and prayers to it,’” said Skeek-Wheeland, remembering some of the posts on social media. “We’re really putting ourselves in a really bad situation.”
Skeek-Wheeland worries that — between Juneau’s population and additional patients possibly coming in from neighboring communities — Bartlett would be quickly overwhelmed.
Skeek-Wheeland isn’t the only one in Juneau asking about Bartlett’s ability to handle a big spike in patients and whether there’s enough equipment on hand.
Like other hospitals around the country, Bartlett has a limited number of ventilators to help seriously ill patients breathe. Fifteen can be used immediately. About two dozen additional machines can be modified to provide oxygen to patients.
But capacity isn’t just a question of the kind of equipment the hospital has available to treat COVID-19 patients. It’s also about where they treat those patients and whether they have enough room.

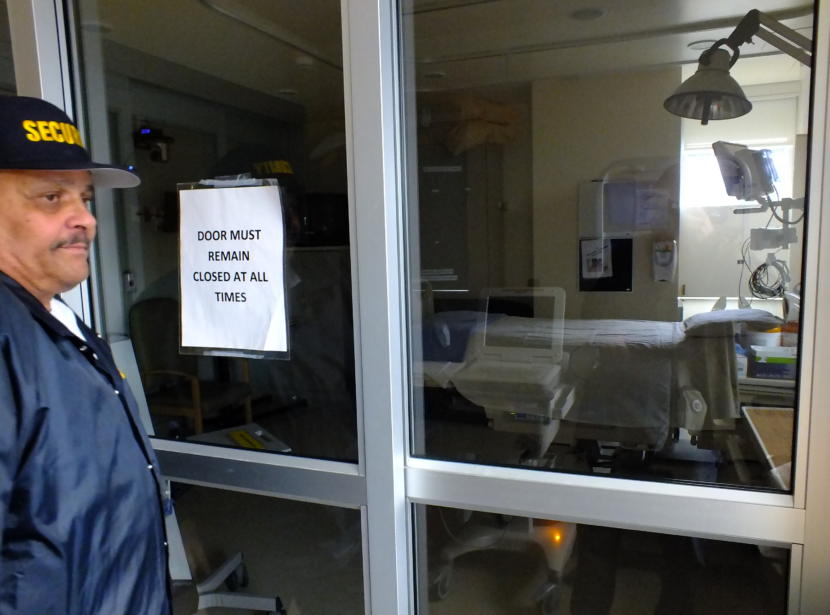
On a floor of the hospital for the most seriously ill patients, there are two special rooms partially enclosed in glass.
“The staff would don their PPE here,” explained Mike Lopez, the emergency management coordinator for the hospital, while standing in the first of the two glass rooms.
“And then here, they would perform patient care on a patient over here,” he said as he opened the door to the second room.
The second room is where a very ill and contagious COVID-19 patient would be treated. This area is specially designed to contain the virus, and to protect other patients and medical staff.
Inside, a whooshing sound comes from air being pulled through high-efficiency filters that remove any contagious airborne viruses.
As Lopez left the patient isolation room and the outer anteroom, a high-pitched tone sounded off.
“Shucks,” said Lopez. “Aw, we just set off the alarm.” The door to the isolation room wasn’t closed entirely.

Elsewhere in the hospital are four specially-ventilated rooms for isolating contagious patients who aren’t critically ill.
Additionally, an entire wing of the hospital has been turned into a temporary isolation ward, with portable filter machines for another eight contagious patients.

Right now, Bartlett is licensed for 56 beds.
But Chief Nursing Officer Rose Lawhorne said they’re preparing to double that.
“We could fit between 90 and a hundred patients in the hospital,” Lawhorne explained.
“And then, we just reviewed our surge plan that would include Rainforest Recovery,” she said. “So, that’s now empty. We could serve another 30-plus patients over there.“
That’s for patients who don’t need critical care or who may be recovering from the coronavirus.
Lawhorne said they also have access to a portable emergency tent hospital that could isolate 16 contagious patients and supply oxygen to another 44.
In total, they could handle 190 patients.
If they still need more space, Lawhorne said they plan on using Centennial Hall or school gyms.
“So we do consider those moments where we don’t like to think about it. You know, the dire circumstances,” Lawhorne said. “We are preparing to care for our friends and neighbors who need us in a situation that we have not seen in our lifetime. And so we’re all working very hard.”
Like Skeek-Wheeland, Lawhorne has been thinking very carefully about the equipment they have and how many patients they can handle at once. That’s why Lawhorne encourages everyone to wash their hands, practice social distancing and stay home.
And there’s a big reason why that message has been drilled into Alaskans over and over again as the virus spreads.
A recent paper by the University of Alaska Anchorage describes how firm shelter-in-place measures enacted by the state and municipalities is the only effective, long-term way to limit the spread of COVID-19. And it’s the way to flatten the curve or spike of infections so that hospitals like Bartlett are not overwhelmed all at once.
