
Dr. Marvin Seppala wrote a book on conquering drug addiction with counseling and group therapy.
The spiritual, abstinence-based strategy pioneered by Alcoholics Anonymous helped him overcome his own alcohol and cocaine addiction when he was 19. As medical director of Minnesota’s fabled Hazelden clinic, he watched it work for patients.
He believed in it — and then he changed his mind.
In 2007, Seppala began working at Beyond Addictions, a now defunct treatment center in Beaverton, Oregon. Instead of relying solely on counseling, the center gave its patients a relatively new medication, buprenorphine, to relieve their drug cravings.
Back in Minnesota, his patients had been bailing out of treatment to use illicit drugs again. In Oregon his patients on buprenorphine weren’t relapsing or overdosing — they reported feeling “normal” again.
Nearly a decade later, doctors and brain researchers agree that medications such as buprenorphine, methadone and naltrexone are the most effective anti-addiction weapons available. Nevertheless, more than two-thirds of U.S. clinics and treatment centers still do not offer the medicines. Many refuse to admit people who are taking them.
The result is that hundreds, perhaps thousands, of Americans are dying unnecessarily, victims of an epidemic that killed more than 28,000 people in 2014 — more than homicides and almost as many as auto accidents.
The research is unassailable: Staying in recovery and avoiding relapse for at least a year is more than twice as likely with medications as without them. Medications also lower the risk of a fatal overdose.
Addicts who quit drugs under an abstinence-based program are at a high risk of fatally overdosing if they relapse. Within days, the abstinent body’s tolerance for opioids plummets and even a small dose of the drugs can shut down the lungs.
And yet as the country’s opioid epidemic worsens — every day, more than 70 Americans die from overdoses, and the numbers are climbing — only about a fifth of the people who would benefit from the medications are getting them, according to a new study by the Johns Hopkins Bloomberg School of Public Health.
“When we discovered medications that worked for AIDS, deaths immediately plummeted. It became a chronic disease instead of a terminal disease,” said Dr. Andrew Kolodny, chief medical officer of the Phoenix House treatment centers, based in New York.
“This epidemic could be the same,” he said. “We have medications for addiction now. But unfortunately, we’re not making them available enough.”
People who could benefit from the medications are not getting them for numerous reasons. Among them:
- Too few health care professionals have specialized training in addiction medicine. Although some primary care doctors have stepped in to fill the void, most are unwilling to treat patients with addictions and say they are often recalcitrant and disturbing to others in their waiting rooms.
- Insurance coverage is limited. Few private insurers and state Medicaid programs cover all of the medications approved by the Food and Drug Administration. When they do, they typically limit the dosage or how long patients can take the medication or require them to first try group therapy, which is cheaper.
- Many leaders of traditional drug treatment centers, such as national detox chains and residential rehab programs, are recovering addicts who conquered their own addictions without medication. They reject the notion that an addict can truly recover from a drug problem by becoming dependent on a different drug.
- Greater use of medication could cut into the centers’ revenue, by reducing the number of people who opt for expensive residential stays. And smaller clinics that might want to add medication services would have to hire a physician to do so, which many of them could not afford.
Dr. Kelly Clark, an addiction specialist in Kentucky and president-elect of the American Society of Addiction Medicine, said some of the resistance is cultural, rooted in a widespread belief “that drug addiction is a moral failing, and that people should just get over it.”
“There is no other disease where approved medications are not provided to everyone who needs them,” Clark said. “We used to consider people with mental illness inferior, even possessed. Scientific advances have combatted stigma around a wide variety of brain diseases, but not addiction.”
Hazelden was one of the many treatment centers that resisted the use of medication — until Seppala returned from his stint in Oregon in 2009 and began pushing the board to shift course. Hazelden started offering the medications shortly thereafter.
“It’s hard to argue when you have patients dying of overdoses,” Seppala said. “We said this is truly a crisis, we can’t just base our service on philosophy, we have to look at the data and base our treatment on the best way to save lives.”
Freedom from Drugs
Opponents say addiction medications such as buprenorphine reduce drug cravings, but they don’t attack the underlying psychological problems that often go with addiction. Nor do they address shame, guilt and self-loathing — as counseling does.
Dr. Robert Mooney’s belief in abstinence has never wavered. As medical director at Vista Taos, a treatment center in New Mexico, he refers his patients elsewhere if they want to take medication. “What we do here is abstinence-based, because there are some people that nothing else will work on,” he said.
Mooney, a psychiatrist and board-certified addiction specialist, beat his own addiction to alcohol and cocaine with an abstinence-based approach, and he grew up in an abstinence-based treatment business. His parents, Dr. John and Dot Mooney, a surgeon and a nurse, overcame their own drug and alcohol addictions through abstinence and opened a treatment center, in Statesboro, Georgia, in 1971, to help others tread the same path.
 “I tell patients, ‘We’re going to take you off all medications and give your brain a chance to land, and it’s going to be a long road.’ You need to prepare people for that.”
“I tell patients, ‘We’re going to take you off all medications and give your brain a chance to land, and it’s going to be a long road.’ You need to prepare people for that.”
Mooney said he isn’t interested in arguing with those who believe in addiction medications, because in his view there has not been adequate research on the long-term effectiveness of either approach. “But let’s at least hang on to an abstinence-based philosophy, because we absolutely need it as part of the solution,” he said.
Seppala’s 2001 book, Clinician’s Guide to the Twelve Step Principles, embraces the approach first laid out in 1935 by Alcoholics Anonymous, “a fellowship of men and women who share their experience, strength and hope with each other that they may solve their common problem.”
He still says addicts who want abstinence-based treatment should get it. But, he said, medication should be offered. Like other addiction doctors, Seppala stresses that medication should be combined with counseling and group therapy whenever possible. Given the horrific toll of the drug epidemic, “We ought to put everyone on some sort of medication and give them all the psychosocial counseling we can,” he said.
The scope of the epidemic is staggering. Since 2008, more than 115,000 Americans have died from overdoses of prescription opioid painkillers and nearly 39,000 have died from heroin overdoses — reaching an overall death rate of 9 per 100,000 in 2014. That’s six times the drug overdose death rate of the 1970s, according to data from the U.S. Centers for Disease Control and Prevention.
New data from the CDC indicate the death toll from this epidemic has not yet peaked. Prescription opioid overdose deaths rose 16 percent from 2013 to 2014, to nearly 19,000. Heroin overdose deaths rose 28 percent and deaths from relatively new illicit opioids, such as fentanyl and tramadol, spiked 79 percent.
According to the U.S. Department of Health and Human Services (HHS), nationwide medication-assisted treatment capacity has increased somewhat in the past decade, but not enough to keep pace with the worsening opioid epidemic.
Many of the nation’s hardest-hit areas are rural and suburban. Rates of addiction are much higher in those areas and the shortage of providers is even worse.
“There are entire communities that are devastated by this epidemic,” Clark said. “If you have an opioid addiction, the odds are good that many, many in your world have the same disease. I’ve treated adolescents and their parents and grandparents.”
Nationwide, nearly 22 million people have some kind of substance use disorder, but only one in 10 goes to a treatment center, according to the most recent survey by the U.S. Substance Abuse and Mental Health Services Administration. In contrast, the treatment rate is as high as 80 percent for other chronic diseases such as diabetes, asthma, heart disease and high blood pressure.
Difficult Terrain
Addiction to opioids, including heroin and prescription pain pills, is difficult to treat. Not everyone recovers. Among those who do, most relapse at least once before entering a period of sustained recovery. For the millions of opioid addicts who are uninsured, homeless or recently incarcerated, getting on medication — and staying on — is a struggle.
But the affluent and the well-educated are also victims of this new epidemic. Their search for effective treatment can be frustrating and dangerous, their relapses frequent.
Kevin Flattery seemed to be in an ideal position to beat his addiction to OxyContin, a widely abused opioid painkiller.
After graduating from the University of Virginia, in 2010, Flattery moved to Hollywood to pursue his passion for filmmaking. Opioid painkillers were cheap and easy to acquire on the street there. Kevin tried them and liked them, in part because they relieved some of the stress he was experiencing as he pursued his high-pressure career.
Two years later, he realized he had an addiction that was taking over his life. Kevin decided to move back to his parents’ home in Mount Vernon, Virginia, an upper-middle-class suburb of Washington, D.C., to find help.
He had family support, financial means and no shortage of local treatment providers. But he got conflicting signals from the counselors he saw.
He checked himself into Inova Fairfax Hospital for detox, and the experts there suggested he start taking buprenorphine, one of the FDA-approved drugs.
The medication worked well for Kevin — at first. But he veered off course a couple of times, stopping the daily medication and buying OxyContin to get high. Each time, he got himself back on buprenorphine within a few days.
Experts say that’s a typical path for people who take such medicines. It often takes several tries before they stabilize and enter a period of sustained recovery.
But after a few months, Kevin wasn’t sure he wanted to stay on the medication for the long term. He attended local 12-step programs where he was criticized for taking it.
Kevin’s father, Don Flattery, said his son was confronted with judgment and pressure about it. “He was made to feel that he was not in recovery, not serious about his sobriety, and substituting one addiction for another — all utterly false but damaging to him nonetheless.”
Conflicted about how to proceed, Kevin stopped taking buprenorphine. Ten days later, he relapsed and suffered a fatal overdose, at age 26.
Three Medications
Buprenorphine and methadone are regulated as controlled substances by the U.S. Drug Enforcement Administration (DEA). Like the opioid painkillers that cause the addictions they are meant to relieve, both are commonly sold on the street.
But their euphoric properties are limited, making them poor options for getting high. The illicit use of methadone can cause a fatal overdose, particularly when combined with other drugs. But buprenorphine is relatively safe, even when used illicitly.
Methadone can cost less than $5 per day; buprenorphine costs about $10 per day. Although medical research has yet to establish standard lengths of time for using either, many have maintained recovery for decades on methadone. Buprenorphine has been used successfully for years by some, and only months by others.
A 2000 federal law requires doctors to seek a special waiver from the DEA to prescribe buprenorphine and limits their number of patients to 30 in the first year and to 100 in subsequent years. HHS may loosen the patient limit this year.
Methadone can only be dispensed by about 1,400 licensed clinics nationwide, both stand-alone and in prisons or hospitals. Most of them are in major cities, meaning the medication is unavailable to most in rural areas. Patients must show up every day to receive their dose under the supervision of a licensed professional.
Vivitrol, an injectable form of naltrexone, is not a narcotic and therefore not regulated. Instead of fulfilling the addicted brain’s perceived need for opioids, it blocks the effect of the drugs and thereby reduces cravings.
 Any doctor can prescribe and administer Vivitrol. But it has a major drawback: To avoid severe and dangerous withdrawal symptoms, patients must completely detox from all opioids for at least seven days before receiving the first shot. For many, that means residential treatment, which can be costly. The drug itself is also expensive, at $1,000 per month.
Any doctor can prescribe and administer Vivitrol. But it has a major drawback: To avoid severe and dangerous withdrawal symptoms, patients must completely detox from all opioids for at least seven days before receiving the first shot. For many, that means residential treatment, which can be costly. The drug itself is also expensive, at $1,000 per month.
Research on Vivitrol’s long-term effectiveness is still to come, but its use is spreading, particularly in jails and prisons. Patients are also increasingly opting for Vivitrol because the shots are effective for 30 days, tempering the temptation of stopping daily doses to get high.
Addiction doctors agree that all three medications should be available to patients, because one may be more effective than another, depending in part on the person’s age, length of time as an addict, home and work environment and underlying mental health issues. The American Medical Association, the American Academy of Addiction Psychiatry and the American Society of Addiction Medicine unequivocally support their use.
Patients should have a say in the kind of medication they want to receive, said Dr. David Gastfriend, scientific adviser to the Treatment Research Institute, in Philadelphia, which analyzes the effectiveness of addiction treatments. “They’ve heard about certain drugs from their friends or they’ve had past experiences and they often have ideas about what they want,” he said. “Treatment works much better with patient buy-in.”
Gastfriend and other addiction experts emphasize that medication should be accompanied by at least some counseling or group therapy. How long patients must stay on the medications remains unknown.
A Turning Point?
For advocates of medication-based treatment, recent policy changes are cause for optimism. The Affordable Care Act allows states to expand health insurance coverage to low-income adults and, for the first time, makes Medicaid and private insurance coverage of substance abuse treatment mandatory.
In the past, Medicaid only covered low-income pregnant women, children and disabled adults. Any drug or alcohol coverage was limited to those three populations. A severe drug or alcohol addiction, while debilitating and life-crushing, did not qualify on its own as a disability.
Under the ACA, 30 states plus D.C. have opted to expand Medicaid to low-income, able-bodied adults, giving millions of poor Americans coverage for addiction treatment. The health law also requires all state Medicaid programs and all insurance companies to cover the gamut of recommended treatments for addiction.
In addition, the federal Mental Health Parity and Addiction Equity Act, although not enforced everywhere, requires insurers to pay for proven addiction treatments at the same dollar level as medical and surgical treatment for purely physical diseases such as cancer.
“There has never been a better time to confront the addiction problem we have in this country,” said Michael Botticelli, director of the U.S. Office of National Drug Control Policy.
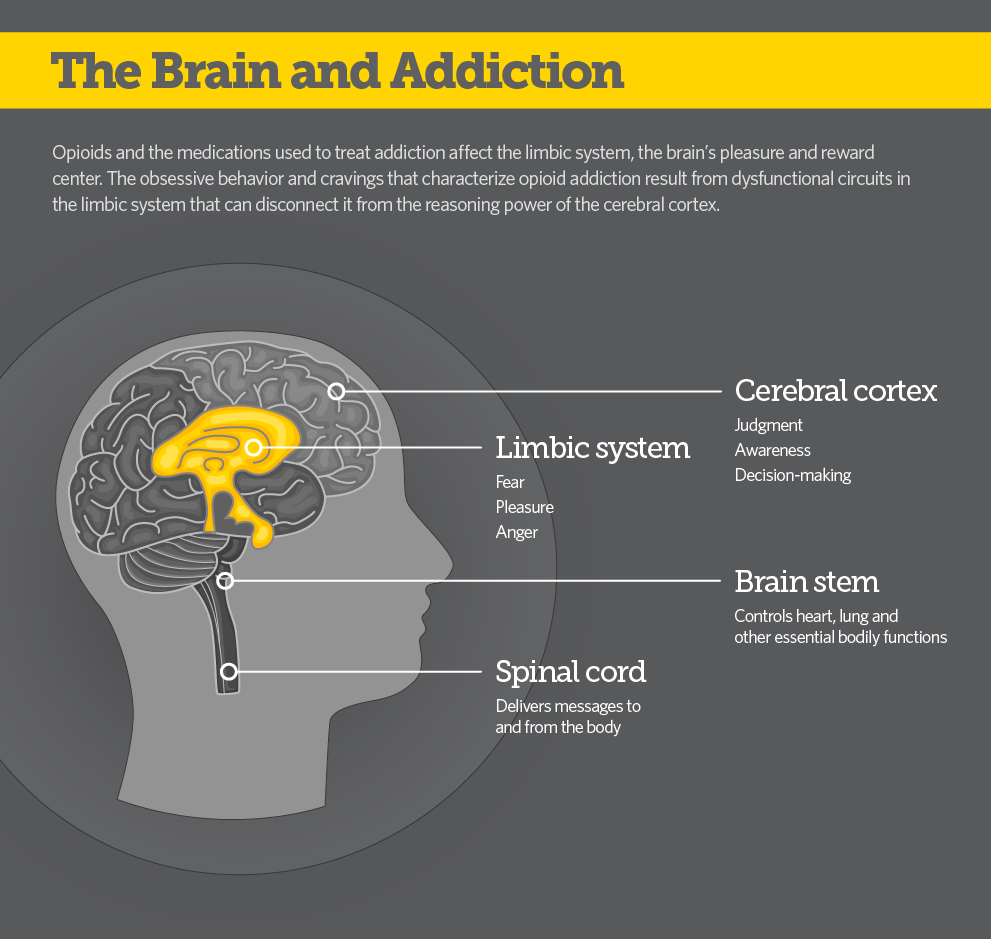
“We know so much more about addiction from years of scientific research. We know that substance use disorders are diseases of the brain, that they can be chronic and relapsing,” Botticelli said. “But we also know that like other diseases, they can be prevented, treated and people can recover.”
Read original article – Published January 11, 2016
In Drug Epidemic, Resistance to Medication Costs Lives
